Indications for APRV ventilation
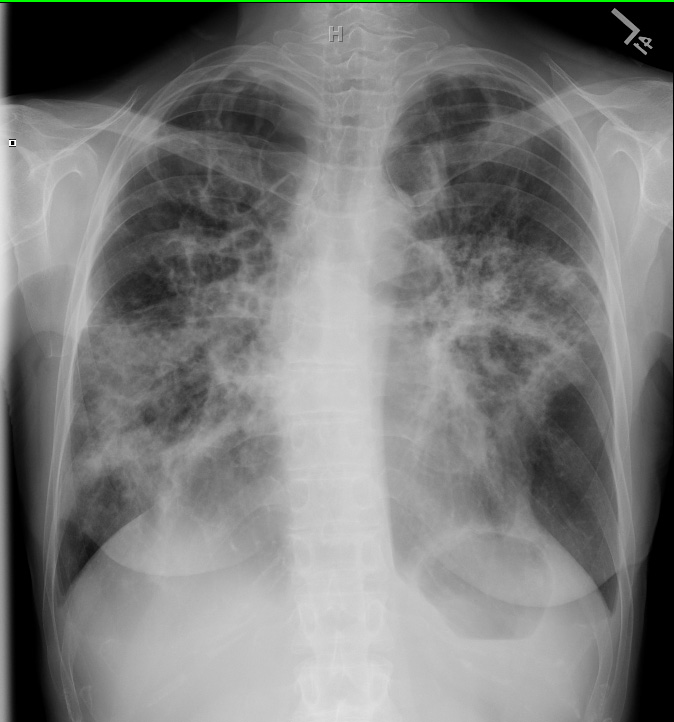
- Acute lung injury (ALI/ARDS)
- Diffuse pneumonia
- Atelectasis requiring greater than 50% FiO2
- Tracheo-esophageal fistual
Initial APRV Settings
- PHigh at the PPlateau (or desired PMean + 3 cmH2O). If your are switching to APRV from a different mode, then PHigh can be set at the previous mean airway pressure. A good starting level would be 28 cmH2O. Higher transalveolar pressures recruit additional alveoli, but, try to keep PHigh below 35 cmH2O.
- THigh at 4.5-6.0 seconds. This is the inspiratory time. The respiratory rate should be 8 to 12 breaths per minute — never more.
- PLow at 0 cmH2O to optimize expiratory flow. The large pressure ramp allows for tidal ventilation in very short expiratory times.
- TLow at 0.5-0.8 seconds. The expiratory time should be short enough to prevent derecruitment and long enough to obtain a suitable tidal volume. A tidal volume target is between 4 and 6ml/kg. If the tidal volume is inadequate, the expiratory time is lengthened; if it is too high (>6ml/kg) the the expiratory time is shortened.
- Automatic tube compensation (ATC) should be on if spontaneously breathing.
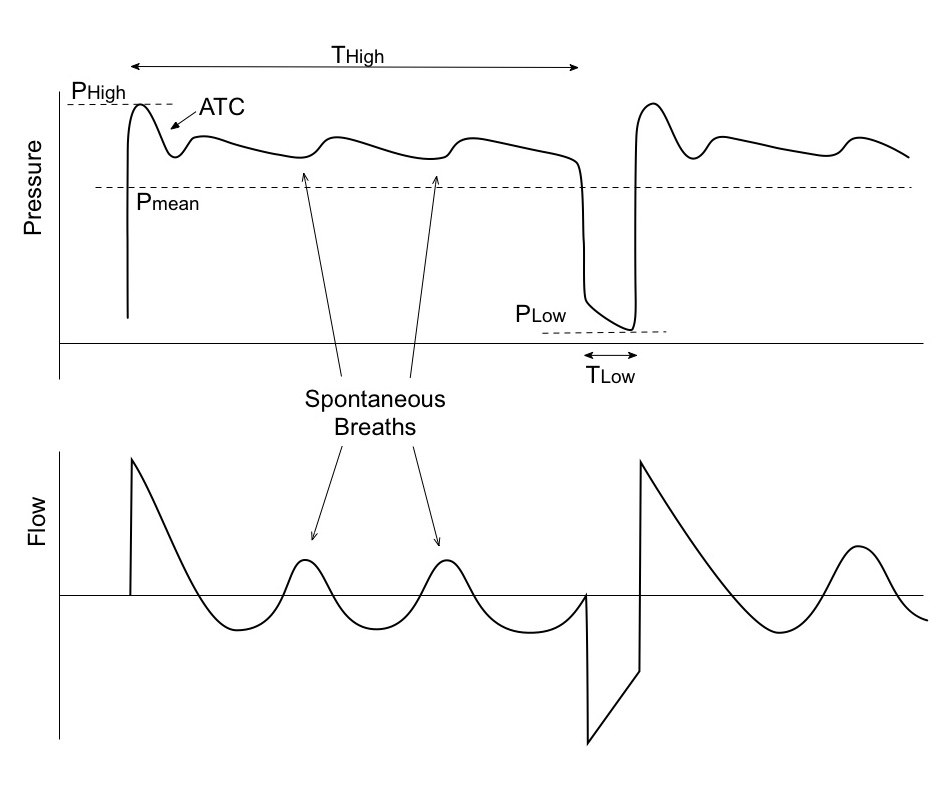
Like Pressure Control-Inverse Ratio ventilation (PC-IRV), APRV utilizes a long “inspiratory time” (THigh) to recruit alveoli and optimize gas exchange. The open exhalation valve allows for spontaneous breathing during THigh.
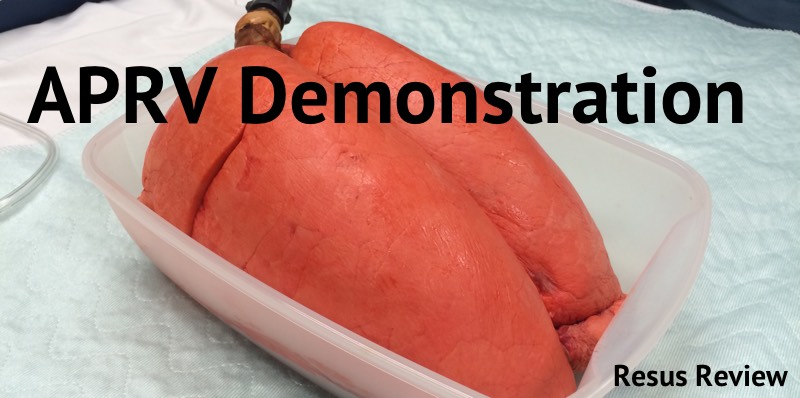
Demonstration of APRV using live pig lungs.
Monitoring a patient on APRV
APRV should help rest the inspiratory muscles and utilize the diaphragm. Once the initial settings are applied, look for anterior chest muscles to be used much less and the diaphragm to be doing the majority of the work. This should occur within hours after placement on APRV. The patient should be breathing more comfortably as recruitment occurs.
The earlier APRV is used, the more effective it is in recruiting the lung and the more likely it is to be tolerated. if initiating APRV late in the course of ARDS, patients sometimes will not look comfortable despite optimal aPRV settings, and they may need an alternative mode.
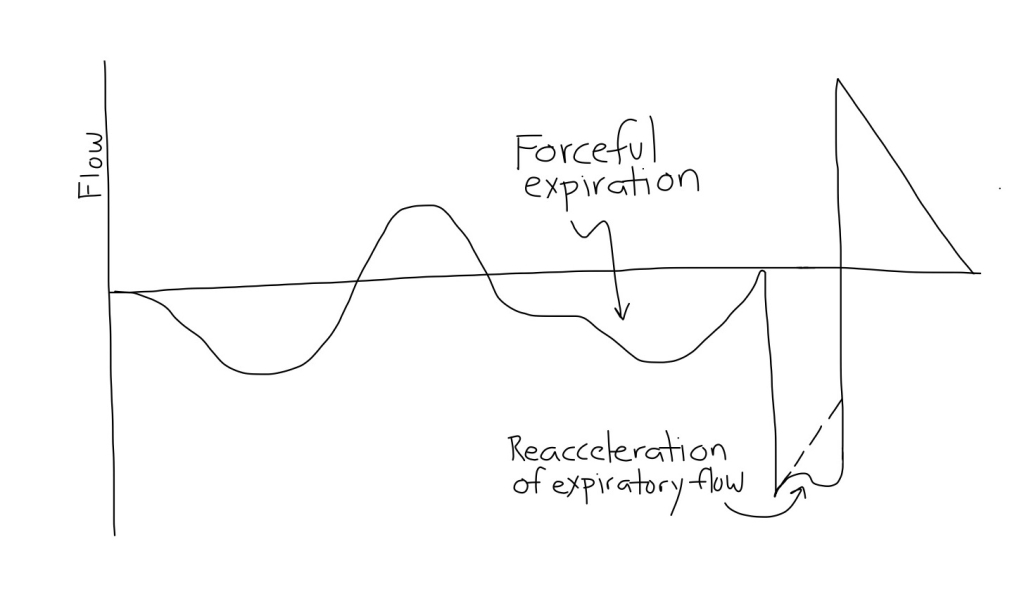
APRV Flow-Time Waveforms
It is important to observe the Flow-Time waveform to optimize the settings. During the pressure release phase, the patient will exhale passively. Adjust the TLow to cut off the expiratory flow during a release at about 50% (25-75%) of peek expiratory flow rate (PEFR).
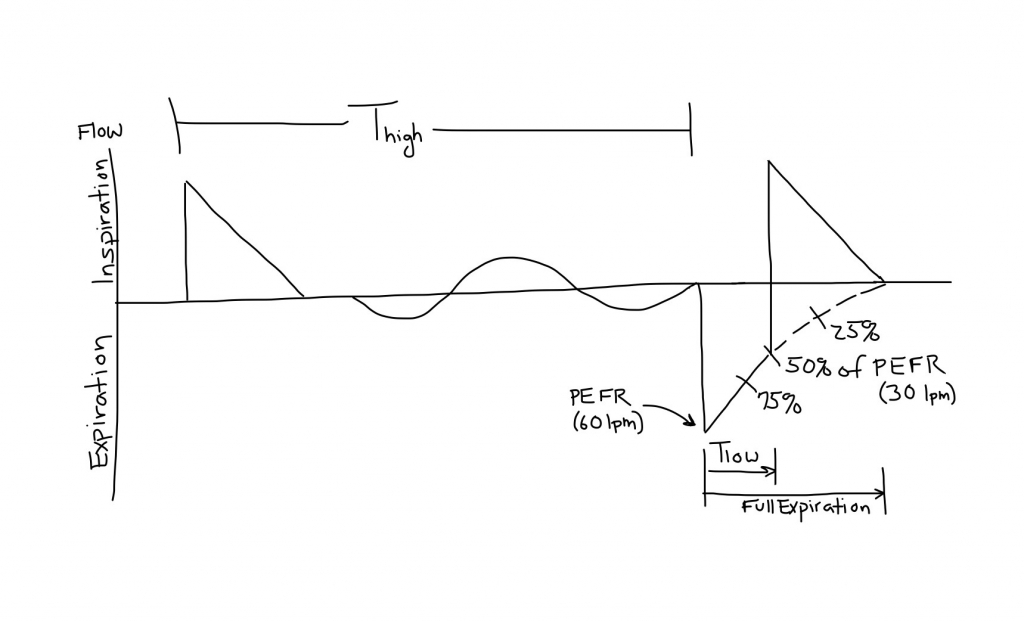
- Never allow the termination of expiratory flow to go <25% of PEFR. This intentional intrinsic PEEP allows PLow to be set at 0 cmH2O without causing derecruitment.
- Generally, the TLow can be as short as 0.3 seconds (closer to 75% of PEFR) in restrictive disease and as long a 1.5 seconds (closer to 25% of the PEFR) in obstructive states.
Making Adjustments to the APRV Settings
Oxygenation Options
- When possible wean FiO2 to <50% for a SpO2 >90% or a PaO2 >60 torr.
- To improve oxygenation via higher PMean:
- Increase PHigh in increments of 2 cmH2O.
- Decrease TLow to be closer to 75% PEFR.
Respiratory Acidosis
- Increase PHigh (up to 40 cmH2O).
- Increase THigh (if spontaneously breathing) in increments of 0.5 seconds up to 8 seconds. If PaCO2 increases with this change, it may reflect inadequate lung volume. If this is the case, try increasing PHigh to re-establish an adequate FRC.
- Increase TLow to allow more time for alveolar emptying, but only if the expiratory flow of a realease doesn’t drop below 25% of the PEFR.
- If further increases in THigh fail to drop PaCO2, you may need to do the opposite: Decrease THigh to increase the rate of releases. This will decrease the PMean and oxygenation. This will then also increase PHigh to maintain the PMean. Maximize PHigh and release rate up to 30 (more like PC-IRV).
- If unable to manage the acidosis with APRV, the mode may be changed to PCV attempting to maintain the same rate and PMean.
Respiratory Alkalosis
- Decrease PHigh (SpO2 may decrease).
- Increase THigh to decrease the release state.
- Turn ATC off if no spontaneous respirations.
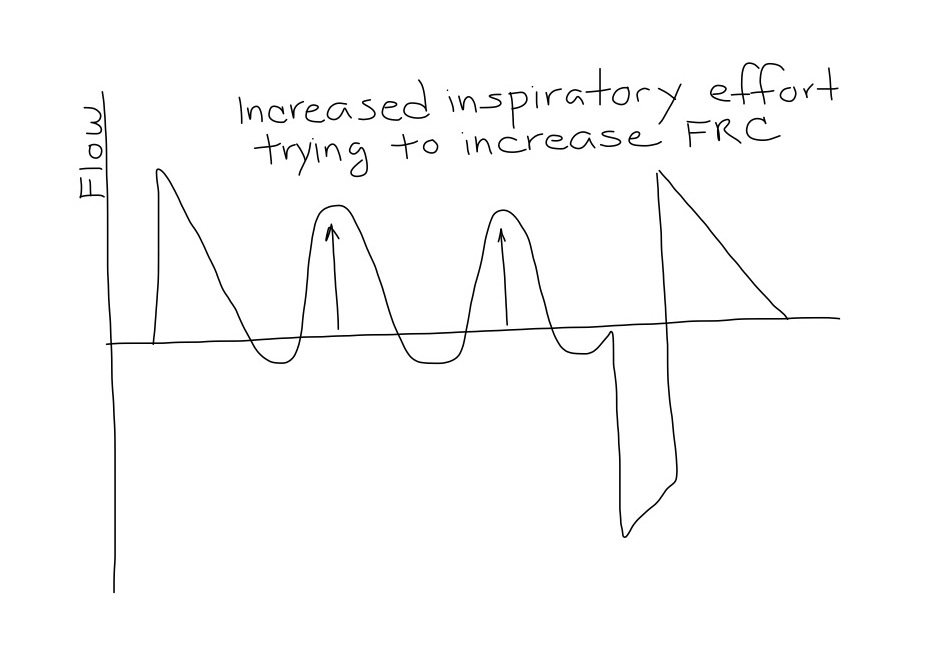
Increased Respiratory Efforts
- If the patient is consistently inhaling forcefully with accessory muscles, they may need alveolar recruitment. Options are:
- Increase PHigh. This will elevate the PMean and encourage recruitment.
- Decrease TLow only if you can maintain the flow during the release phase <75% of PEFR and the PaCO2 and pH are acceptable.
Forceful expirations
- If the patient seems to be exhaling forcefully, over-inflation may be present. Options are:
- Decrease the PHigh in 1-2 cmH2O increments and increase THigh (to maintain the same PMean).
- Increase the TLow. Allowing more time to exhale only if you can maintain the flow during the release phase >25% of PEFR.
- CXR should be monitored for lung over-inflation.
APRV Weaning
When FiO2 is titrated below 50%, recruitment is maximized and the patient is breathing spontaneously, a continuous gradual wean can begin by:
- Decreasing the PHigh by 1-2 cmH2O and increasing the THigh by 0.5 seconds for every 1 cmH2O drop in PHigh. This is referred to as the “drop and stretch”.
- “Drop and stretch” should be done every two hours or more if tolerated. As you “drop and stretch” the PMean is gradually lowered, so you will need to monitor SpO2. Changing the CPAP or dropping PMean too quickly will possibly de-recruit alveoli.
- Throughout the weaning process, the patient should be closely monitored for increasing work of breathing, tachypnea, or a drop in SpO2. If this occurs, return to the previous settings.
- When the PHigh reaches 10 cmH2O and the THigh reaches 12-15 seconds, change the mode to CPAP with PEEP at 10 cmH2O and pressure support at 5-10 cmH2O. ATC should be off. Slowly wean CPAP was tolerated.
- The patient should be spontaneously breathing throughout this process, therefore it is not necessary to do spontaneous breathing trials.
References
- CritCareMed. 2005;33:S228 Other Approaches to Open-Lung Ventilation–Airway Pressure Release Ventilation.
- CleveClinJMed 2011;78:101 Airway Pressure Release Ventilation–Alternative Mode of Mechanical Ventilation in Acute Respiratory Distress Syndrome.
- AnnThoracMed 2007;2:178 Airway pressure release ventilation.
- AACNClinicalIssues 2001;12:234 Airway Pressure Release Ventilation–Theory and Practice.

Good work!
Do you have any references about APRV to share?
Thanks
Thank you for this! This is an invaluable resource for the EM/CC provider. Great work!
[…] provides us with a nifty Resus Review on the APRV Ventilation Mode — Introduction, Basic Use, Management, and Advanced Tips – worth a gander for those that are unfamiliar with it… and for those who […]
This is an excellent review, thank you! I do have a question though, how does this not lead to auto-PEEP? Based on the flow diagram you showed setting your Tlow to >25% PEFR seems like it would lead to breath stacking and auto-PEEP, which could result in tension physiology.
Because PEEP low is set at 0 you need autopeep to prevent alveolar collapse
define bilevel mode
bilevel is equal to aprv what you say
Bilevel (e.g Puritan Bennett ventilators) is the same as bipap ventilation (e.g. Drager?). Essentially two levels of CPAP (Phigh and Plow cycle for Thigh and Tlow respectively) where the mechanics of the ventilators are such that spontaneous breathing is entirely easy at both CPAP levels.
APRV is a subset of bilevel (or bipap) ventilation where the ‘constraints of the subset is 0.3s<=Tlow<=1.5s
BiVent mode (Servo-I) is equal to APRV
Bilevel (e.g Puritan Bennett ventilators) is the same as bipap ventilation (e.g. Drager?). Essentially two levels of CPAP (Phigh and Plow cycle for Thigh and Tlow respectively) where the mechanics of the ventilators are such that spontaneous breathing is entirely easy at both CPAP levels.
APRV is a subset of bilevel (or bipap) ventilation where the ‘constraint’ of the subset is 0.3s<=Tlow<=1.5s
RECENTLY WE HAD A PATIENT COPD & H1N1 Pneumoniae leading to ARDS , APRV sent him to very high levels of PC02 respiratoryacidosis we had to go back to pressure ventilation with small volumes and low frecuency 16 with I:E 1 to 4 and low PEEP 10 cms. to be able to correct his severe acidemia
Dear Alvaro APRV in general is contraindicated for APRV as COPD patients require long expiratory time (Te).
You are a great mind. Thanks for the info.
Jim
Nice job, you explained APRv
Jvery well. This keeps my edge very sharp. I love being a reapiatory therapist. We have a great profession, because of the people in our profession. I am proud to with these respiratory professional. Thank you.
Is there anyway I can extract the video that is showing the lungs to use in a powerpoint presentation?
Feel free to contact me to obtain videos and permission.
Great article. I wonder if we might chat about this for my podcast ‘Critical Care Practitioner’. I think both myself and my audience would appreciate your insights into this topic.
great post. Could you explain How increase in T low increases tidal volumes?
Thank you for your valuable contributions.
[…] Please find a summary and video resource by Resus Review on Airway Pressure Release Ventilation (APRV) […]
[…] APRV Ventilation Mode — Introduction, Basic Use, Management, and Advanced Tips – Resus Review […]
Awesome article with an objective affect. The problem I see in my hospital is the “Intensivists” know a little about APRV and don’t quite master its implementation and application. When the patient starts to go “South”, a few of them think that more is better and simply begin to increase settings. We’ve had to go in and salvage those scenarios several times. Frustrating!!!