A 45-year-old man with severe coronary heart disease s/p CABG but with an unprotected left main, presented to the emergency department for evaluation and suffered a ventricular fibrillation cardiac arrest. CPR and BVM ventilation was initiated immediately. The patient underwent an aggressive resuscitation effort with:
- LUCAS CPR and ResQPod impedance threshold device
- Multiple defibrillations
- Amiodarone
- Magnesium
- Lidocaine
- Esmolol
At this point the patient had received high-quality uninterrupted CPR, electrical defibrillations, inovasopressors, and antiarrhythmics. Despite this, the patient had persistent ventricular fibrillation. Intermittent cardiac ultrasound showed no cardiac activity. What options remain?
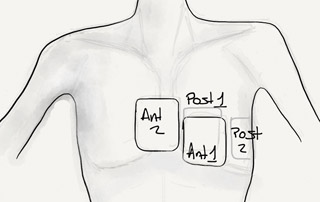
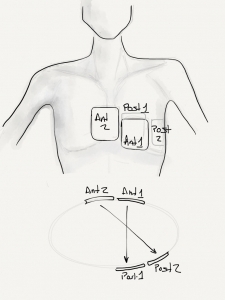
We decided to attempt high energy defibrillation. The use of a second defibrillator with separate pairs of electrodes allows 400 J of biphasic energy to be applied to depolarize a critical amount of myocardium. First described by in animal models by Geddes (4) in 1976, and then by Hoch (1) in 1994. He found that patients who developed refractory ventricular fibrillation during electrophysiology procedures had restoration of regular rhythm.
High energy defibrillation is performed by attaching a second set of pads attached to a second defibrillator, ensuring that a second vector is established through the heart. At the time of defibrillation, both shock buttons are depressed as near-simultaneously as possible.
While the high energy increases the likelihood of successful defibrillation, the severity of postresuscitation myocardial dysfunction increases with the magnitude of electrical energy delivered by the shock (2).
With all of these above efforts including the high energy defibrillation, the patient had brief ROSC, at which point he was taken to the cardiac catheterization lab. However, en route, he became bradycardic again, and LUCAS CPR had to be restarted. Angiography was performed with ongoing CPR, which showed a complete left main thrombosis. A thrombectory was performed and TIMI III flow was restored. We considered initiating extracorporeal membrane oxygenation, however, it was apparent that despite restoration of coronary flow, the patient had no sustaining rhythm. He had pulseless electrical activity, that was not perfusing.
References:
- Hoch et al. “Double sequential external shocks for refractory ventricular fibrillation.” Journal of the American College of Cardiology. April 1994. 23(5): 1141.
- Xie et all. High-Energy Defibrillation Increases the Severity of Postresuscitation Myocardial Dysfunction. Circulation 1997;96:683.
- Walcott et al. Comparison of low-energy versus high-energy biphasic defibrillation shocks following prolonged ventricular fibrillation. Prehospital Emergency Care 2010;14(1):62.
- Geddes et al. The increased efficacy of high-energy defibrillation. Medical and biological engineering 1976;14(3):330.

[…] We have discussed the option of using high energy defibrillations. […]
[…] Charles Bruen has a great post with the evidence […]
[…] High Energy Defibrillation for Incessant Ventricular Fibrillation on Resus Review […]
I just had a successful use of dual defib. 22 year old male, PMG WPW with successful ablation 10 years prior. Sudden collapse in front of friend, no exertion, no prodrome. ACLS by EMS, refractory VF despite defib, epi, amiodarone. In ER he got 1 more shock then I emplyed dual defib x 1. Initial wide perfusing rhythm then to sinus rhythm. Transferred to tertiary care. DC to home 3 weeks later with CPC 1!!!!!
That is an awesome use of the technique. Nice save by your team!